Tele-expertise is a digital tool in full expansion in the field of health, facilitating collaboration between general practitioners and specialists. It is up to you to seek the opinion of a colleague expert, remotely, to optimize the care of one of your patients. This practice fits perfectly into the framework of telemedicine, and has many advantages for you, health professionals, both in terms of quality of care and organizational efficiency.
In this article, we will explore the benefits of tele-expertise in detail, highlighting its positive impacts on medical practice, interprofessional collaboration, and access to care for patients.
I. Improving the quality of care
Tele-expertise makes it possible to quickly obtain the opinion of a specialist in complex situations or situations requiring specialized expertise. This leads to a better quality of care by ensuring more accurate diagnoses and better adapted treatments.
- Fast access to specialized expertise : By seeking the advice of a specialist via tele-expertise, you can refine your diagnosis or adjust the treatment plan without having to organize a physical appointment. This reduces patient wait times and improves care, especially in situations where speed is critical.
- Reducing medical errors : Tele-expertise makes it possible to limit errors related to diagnostic uncertainties. Seeking a specialized second opinion improves the accuracy of the diagnosis, which reduces the risk of inappropriate treatment.
II. Reducing inequalities in access to care
Tele-expertise plays a key role in reducing regional disparities in access to specialized care, especially in rural or under-medicalized areas.
- Improving access to specialists in rural areas : Patients in rural areas or areas far from major medical centers benefit from faster and easier access to specialized care, without having to travel. Tele-expertise allows you to consult experts located hundreds of kilometers away, thus ensuring a level of care equivalent to that of large cities.
- Avoid expensive and tiring trips : Tele-expertise makes it possible to limit trips to specialized centers, often far from patients' homes. This is particularly beneficial for the elderly, those with chronic illnesses or those with reduced mobility, who can receive specialist advice without leaving their homes or cities.
III. Optimizing interprofessional collaboration
Tele-expertise promotes a fluid and rapid exchange between the various health professionals, improving the coordination of care around the patient.
- Strengthened collaboration between doctors : By facilitating communication between general practitioners and specialists, tele-expertise establishes a real collaborative dynamic. Generalists can consult specialists quickly and easily, while specialists can share their expertise without being overwhelmed by unnecessary in-person consultations.
- Ongoing knowledge exchange : For general practitioners, tele-expertise also represents an opportunity to learn and refine their skills through regular exchanges with specialists. This contributes to the continuous improvement of medical practices and knowledge.

IV. Time and efficiency savings for doctors
Tele-expertise makes it possible to better manage medical time, by optimizing consultations and by reducing unnecessary travel.
- Reduction in unnecessary physical consultations : By obtaining specialized advice remotely, the attending physician can avoid referring a patient for a face-to-face consultation that could prove useless. This makes it possible to unclog specialized offices, while reducing the flow of patients in hospitals and care centers.
- Reduction of treatment times : The time required to get an appointment with a specialist is often long. Tele-expertise makes it possible to speed up the process, offering an opinion in a few hours or days, compared to several weeks or even months for a face-to-face consultation. This is particularly beneficial for pathologies that require rapid treatment.
V. Improving the continuity of care
Tele-expertise fits perfectly into a care path where continuity is essential, especially for patients suffering from chronic diseases or requiring regular follow-up.
- Optimized follow-up for complex patients : For patients with complex pathologies or requiring the intervention of several specialists, tele-expertise makes it possible to coordinate care more effectively. Doctors can visit specialists regularly to adjust treatments according to the evolution of the disease.
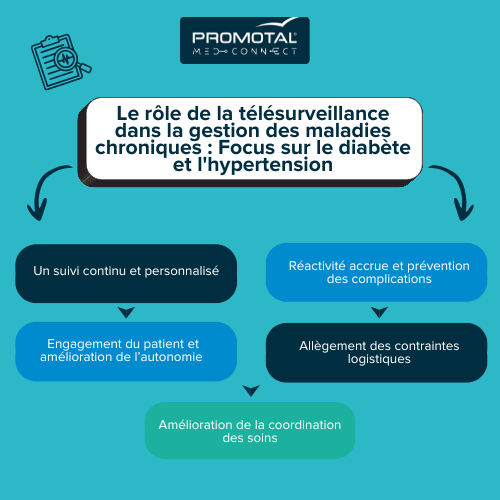
- Remote monitoring of chronic diseases : Patients suffering from chronic diseases such as diabetes or hypertension benefit from closer and continuous monitoring thanks to tele-expertise. The general practitioner can consult an endocrinologist or cardiologist without requiring a physical appointment for each treatment adjustment.

VI. Reduced costs for patients and the healthcare system
Tele-expertise contributes to reducing costs for both patients and the health system, while maintaining a high quality of care.
- Fewer costs for patients : By avoiding unnecessary physical consultations with specialists, patients save on the costs associated with travel, medical leave, or accommodation costs, especially for those living far from health centers.
- Streamlining medical resources : On the health system side, tele-expertise makes it possible to better allocate resources by focusing face-to-face consultations on cases that really require a physical assessment. This frees up consultation slots for urgent or more complex situations.

VII. Conduct of a tele-expertise consultation
Here are the main steps of a tele-expertise consultation:
1. Identifying the need for expertise
The tele-expertise process starts when you identify a case that requires additional advice or expertise. This may be due to a number of reasons:
- A complex or rare pathology
- Diagnostic uncertainty
- The need for confirmation on a treatment
- The need to adapt a care plan or to assess the evolution of a chronic disease
2. Transmission of medical information
Once the need for expertise has been identified, you collect the information necessary for the specialist to properly understand the case. This information generally includes:
- The patient's complete medical file (medical history, history, etc.)
- The results of the examinations carried out (laboratory analyses, X-rays, X-rays, MRIs, ultrasound, etc.)
- Relevant clinical data (symptoms, clinical signs, disease progression)
This information is transmitted via a secure telemedicine platform, which guarantees the confidentiality of patient data in accordance with current security standards.
3. Analysis by the specialist
Once the medical information is transmitted, the specialist analyzes the data and documents provided. Depending on the case, it may be a specialist in cardiology, neurology, neurology, dermatology, radiology, or any other field concerned with the problem raised.
The specialist may also ask for further details or examinations if the data provided is not sufficient to establish an informed opinion.
4. Rendering of the medical opinion
After analyzing the information, the specialist writes his medical opinion. This notice may include:
- An accurate diagnosis or confirmation of the initial diagnosis
- Therapeutic recommendations (adjustment of treatment, change of medication, etc.)
- A suggestion for the management of the patient (referral to another specialist, need for additional examination, etc.)
The opinion is sent to you via the tele-expertise platform. You remain responsible for communicating the findings to the patient and implementing the recommendations.
5. Follow-up and implementation of recommendations
Finally, you will read the opinion given by the specialist and integrate it into the patient's care. If the specialist's opinion involves adjustments in treatment or new examinations, you should inform the patient during a consultation or remote follow-up.
Tele-expertise can be used in the context of monitoring chronic diseases or complex pathologies. If necessary, you can request new expertise as the patient's condition evolves.
6. Traceability and documentation
Each stage of the tele-expertise consultation is documented and archived in the patient's medical file, which guarantees complete traceability of exchanges and decisions taken. It also facilitates a possible follow-up or return to the specialist if the patient has an unexpected change in his health condition.
Specific cases: Real-time vs asynchronous tele-expertise
Tele-expertise can take place in two different ways:
- Asynchronous tele-expertise : In this case, the specialist analyzes the data and gives his opinion at a later time. This does not require the applicant and the expert to be available at the same time. This is the most common form and is particularly suitable for exchanges where speed is not essential.
- Synchronous tele-expertise (in real time) : It takes place as a direct exchange between the attending physician and the specialist, sometimes in the presence of the patient or with data transmitted in real time (ultrasound images, instant examination results). This type of expertise is often used for urgent situations or cases requiring immediate intervention.
Conclusion
Tele-expertise is proving to be a valuable asset for health professionals. It improves the quality of care through rapid access to specialized advice, reduces inequalities in access to care, optimizes collaboration between doctors, and allows more effective management of resources and time. In addition, by facilitating the care of complex patients and speeding up diagnostic processes, it contributes to better continuity of care while reducing costs for patients and the health system.
Although physical consultation is still necessary for some cases, tele-expertise is an essential complement to modern medical practice, making it possible to respond more effectively to the needs of patients and professionals in an increasingly connected world. It paves the way for more collaborative, more accessible, and more responsive medicine.

.png)
.png)